Glaucoma
Glaucoma
Congenital Glaucoma
This is an uncommon disease affecting the newborn with an incidence of about 1:10,000. It may occur as an isolated condition or in the setting of associated systemic abnormalities.
It may involve one or both eyes. Once identified, the condition is primarily managed at a tertiary institution ie Perth Children’s Hospital. It can present as clouding of the cornea which also appears larger than usual (buphthalmos), epiphora (watery eye), photophobia (light sensitivity).

Examination under anaesthesia (EUA)

Cyclodiode-photocoagulation of ciliary body
The topic is vast and complicated, below is a link for those interested to read further.
https://www.aao.org/topic-detail/congenital-glaucoma-asia-pacific
Glaucoma in adults poses a different perspective in management. Causes are varied and multifactorial. Risk factors may include: Age over 60, raised intraocular pressure (IOP), ethnic background (black African descent, Hispanics, Asians), family history, eye trauma, hyperopia, myopia, prolonged steroid use, diabetes, migraine
In essence, the intraocular pressure of the eye is often (not always) raised with resultant damage to the optic nerve(s) and subsequent visual loss, starting usually from the periphery.
Ocular Hypertension is a term applied to individuals where the intraocular pressure is high and requires treatment but with NO evidence of nerve damage and field loss. However, left untreated, there would be increase risk of developing glaucoma.
Bear in mind that the intraocular pressure (IOP) is just an approximate measurement and is never accurate regardless which device is used. The triad of raised IOP, typical disc cupping and supporting visual field loss supports the diagnosis of glaucoma.


Both disc photos showing inferior disc margin thinning with associated nerve fiber layer loss

Left inferior disc cupping, thinned disc margin with corresponding superior field loss
The aim of management fundamentally is to reduce the IOP as low as possible. This is achieved by means of either topical drops, use of laser (Selective Laser Trabeculoplasty or Argon Laser Trabeculoplasty) or glaucoma filtering surgery with various types of shunts available.
Glaucoma filtering surgery will be the last option when all else fails to control the intraocular pressure. The gold standard of trabeculectomy still stands as a robust surgery with or without augmentation with anti-metabolites and various types of shunts.
With trabeculectomy, a tiny tissue flap on the sclera is fashioned (like a trap-door) which allows the aqueous (fluid within the eye) to seep out slowly with the aim of dropping the intraocular pressure.
I usually insert an Ex Press shunt into the anterior chamber placed beneath the scleral flap. There are various types of shunts available to date and the choice of shunt will vary between surgeons and experience. The fluid collects beneath the conjunctival, forming a bleb (blister) as shown in this photo.
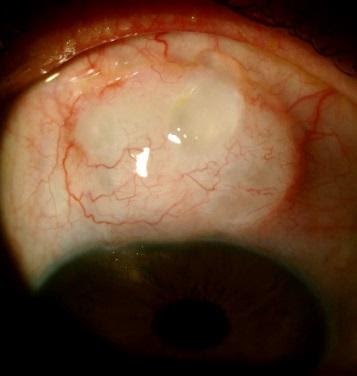
a functioning filtering bleb
The problem is normal healing process will form a scar, which will ‘close’ that trap-door or scleral flap. It is necessary to perform ‘needling’ with a needle to break up the scar tissue overlying the scleral flap, performed under topical anaesthetic in the office; with injection of an anti-metabolite eg. 5-Fluorouracil (5-FU), aiming to reduce inflammation and scarring.
The progress can be tedious and prolonged for the patient and can take months before stable intraocular pressure achieved. Sometimes, the surgery fails due to significant scarring where needling is ineffective and repeat surgery deemed necessary. There is no cure for the disease but one aims to slow down disease progression.
It is important that those suffering from glaucoma be monitored regularly by an ophthalmologist. There are many sources of information but below are several links which some may find useful.
https://ranzco.edu/policies_and_guideli/glaucoma/
https://www.aao.org/eye-health/diseases/what-is-glaucoma
https://www.youtube.com/watch?v=vyggkF8R-UQ
https://www.glaucoma.org.au/