Medical Retina
Medical Retina
Broadly speaking, the term medical retina refers to medical diseases affecting the retina, the layer of neural tissue at the back of the eye.

Optic disc is the round / white looking structure and macula is the darker area in the middle of the photo seen left of the optic disc. Macula is the important part of the retina providing your functional central vision and colour vision. They are numerous diseases, many unique to the eye with no systemic association which can cause injury to the retina. Some are seen affecting only the macula while others may affect any part of the retina.
Several common conditions include:
- Age related macular degeneration (ARMD)
The commonest cause of visual blindness in the western world. There are two main forms, dry and wet. The dry form leads to progressive painless central visual loss. Unfortunately, there is currently no cure. The wet form refers to a bleed or leak at the macular area leading to a more rapid visual loss. Once confirmed, there is treatment available by means of an injection of a medication into the eye.
Currently available drugs include Lucentis (ranibizumab), Eylea (aflibercept), Avastin (bevacizumab) and more recently Beovu (brolucizumab).The link below provides a good explanation for those interested to read on.


Diagnosis is often made clinically and usually confirmed with OCT, now less commonly with FFA (fluorescein angiogram) as OCT-A (angiogram) is now able to provide much higher resolution images and details for diagnosis. Intravitreal injection of anti-VEGF drugs is performed under topical anaesthetic in the rooms. The link to eye injections below explains it well.

Left exudative maculopathy (ARMD), pre and post anti-VEGF injection with good response
Links below provide additional source of information for those interested.
https://www.mdfoundation.com.au/content/macular-degeneration-about
https://ranzco.edu/policies_and_guideli/age-related-macular-degeneration-amd/
https://ghr.nlm.nih.gov/condition/age-related-macular-degeneration
https://www.aao.org/eye-health/diseases/amd-macular-degeneration
- Diabetic retinopathy
A microangiopathy affecting the small blood vessels at the back of the eye, the retina. It is estimated that one-third of diabetics have diabetic retinopathy, a leading cause of preventable blindness in this country. It is important for a diabetic to have their eyes examined regularly, usually annually or every 2 years depending on the clinical assessment.
One may not be aware of any eye involvement until the macula is affected (diabetic macular oedema) with resultant reduced central vision or a bleed into the vitreous causing reduced or blurred vision indicating a much advanced stage of the retinopathy.
Depending of the severity, one may see microaneurysms, dot/blot flame haemorrhages, hard exudates, retinal oedema, cotton-wool spots, changes in the caliber of vessels (venous beading) and intraretinal microvascular abnormalities (IRMA).
The longer duration one has diabetes and the poorer control it is, the higher the risk of developing diabetic retinopathy. Complications such as diabetic macular oedema leads to reduced vision and needs to be treated. This involves an injection of anti-VEGF with or without retinal laser.
Bleeding into the vitreous usually comes from abnormal blood vessels formed at advanced stage of the retinopathy and may require surgery ie vitrectomy and laser. It is important to understand that strict stable control of glucose level, hypertension and cholesterol are all important factors in the overall management.
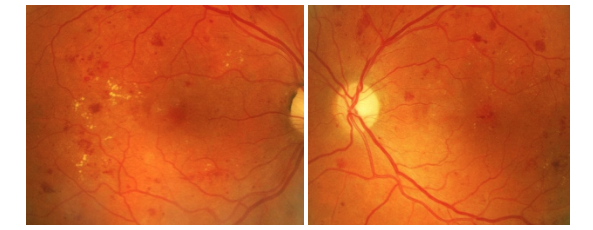
Same patient with bilateral moderate non-proliferative diabetic retinopathy and diabetic macular oedema
- Retinal vein occlusion
The blood supply into the retina comes from one artery (central retinal artery) and leaves via one vein (central retinal vein). However, either part of or the main retinal vein exiting the retina may become blocked, causing bleeding and swelling of the retina with resultant visual loss.

There are many causes and do seem to affect the elderly particularly in the 60’s onwards although it can occur in younger age group.
Various risk factors may include: age, hypertension, diabetes, blood disorders (increased blood cells or increased blood proteins), raised intraocular pressure, optic disc swelling.
Symptoms may be subtle or obvious with partial or complete sudden visual loss, relative field loss, blurring of vision which gets worse over hours or days.
Loss of vision from either branch (BRVO) or central retinal vein occlusion (CRVO) is due to swelling of the maculae ie cystoid macular oedema.
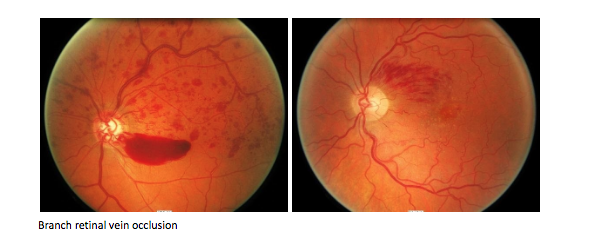
Diagnosis is made clinically and the extend of the macular oedema can be assessed with an OCT, which can provide sequential scan reviews of progression.
Treatment may involve regular observation to retinal laser and intravitreal injection depending of the extend of involvement.
Further complications may arise with recurring swelling of the macula, formation of abnormal blood vessels which can bleed into the vitreous.
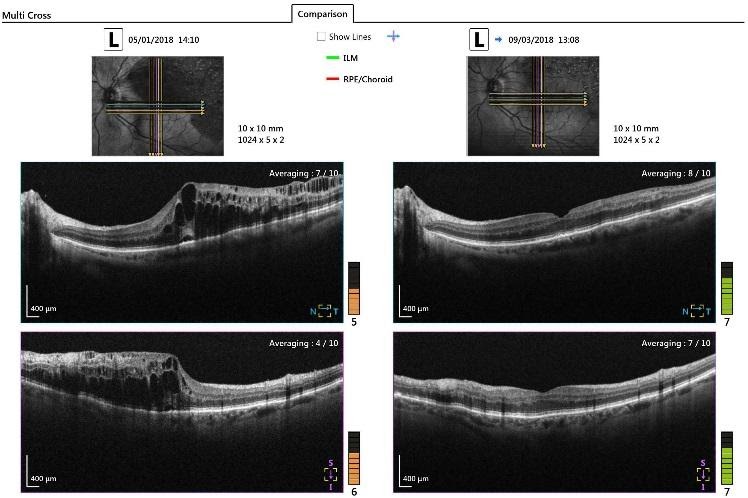
Left column: Left retinal OCT with superotemporal branch retinal vein occlusion and significant cystoid macular oedema
Right column: Post intravitreal anti-VEGF injection with resolution of cystoid macular oedema and retinal swelling
Below are several informative links.
https://mdfoundation.com.au/content/about-retinal-vein-occlusion
https://www.aao.org/eye-health/diseases/what-is-central-retinal-vein-occlusion
https://www.aao.org/eye-health/diseases/branch-retinal-vein-occlusion-treatment
https://www.aao.org/eye-health/diseases/central-retinal-vein-occlusion-diagnosis